A large-scale genetic study involving over 268,000 individuals has revealed a surprising connection between genes involved in vitamin B1 (thiamine) metabolism and gut motility – the process that governs digestion, nutrient absorption, and waste elimination. The findings, published January 20, 2026 in the journal Gut, suggest that variations in how people process thiamine may influence bowel habits and potentially offer new avenues for treating conditions like constipation and irritable bowel syndrome (IBS).
The Complexity of Gut Motility
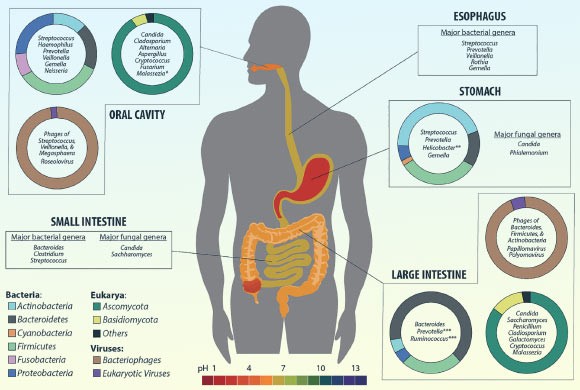
Gut motility is not simply about moving food through the digestive system; it’s a complex interplay between the gut-brain axis, immune function, the gut microbiome, and external factors like diet and medication. Disruptions in this process underlie numerous gastrointestinal disorders, including severe cases of chronic intestinal dysfunction. Pinpointing the exact biological mechanisms behind these disruptions has been a long-standing challenge for researchers.
Genetic Roadmap to Bowel Function
Researchers, led by Professor Mauro D’Amato at LUM University, used genetic data from individuals of European and East Asian ancestry to identify 21 genomic regions influencing bowel movement frequency – 10 of which were previously unknown. The study confirmed previously known pathways, such as bile acid regulation and nerve signaling, but the most striking result centered on genes SLC35F3 and XPR1, which govern thiamine transport and activation.
Thiamine and Bowel Movements: A Real-World Link
Further analysis of dietary data from nearly 98,500 participants showed a correlation between higher thiamine intake and more frequent bowel movements. Critically, this relationship was modulated by genetics. Individuals with specific variations in the SLC35F3 and XPR1 genes responded differently to thiamine intake, suggesting that inherited differences in thiamine handling may play a role in bowel habits.
“We used genetics to build a roadmap of biological pathways that set the gut’s pace,” explained Dr. Cristian Diaz-Muñoz, a researcher at CIC bioGUNE- BRTA. “What stood out was how strongly the data pointed to vitamin B1 metabolism, alongside established mechanisms like bile acids and nerve signaling.”
Implications for IBS and Future Research
The findings also highlight a biological overlap between bowel movement frequency and IBS, a widespread condition affecting millions. The study underscores the need for further research – including lab experiments and clinical trials – to test whether targeted interventions involving vitamin B1 metabolism could improve gut motility and alleviate symptoms of IBS and other related disorders. The study’s findings mark a critical step in understanding the complex biology of gut function.
The study reinforces the idea that personalized medicine will eventually become more widespread: genetic variation plays a role in how our bodies respond to nutrients, and this must be taken into account for optimal health.